Is My Toddler's Walk Normal? Waddling Gait vs. Trendelenburg Gait
Most toddler waddling is normal and disappears by age three. Lurching to one specific side (Trendelenburg gait) signals hip muscle weakness that needs medical attention.
Updated August 11, 2025

Your 18-month-old lurches from side to side like a tiny sailor. They fall constantly. Their legs spread wide with each step.
Is this normal? Or should you worry?
Most toddler "funny walks" are perfectly normal. But some signal real problems that need immediate attention. If you're looking for waddling gait vs. Trendelenburg differences, this guide shows the clear signs and next steps
Trendelenburg Gait vs Waddling Gait (Quick Summary)
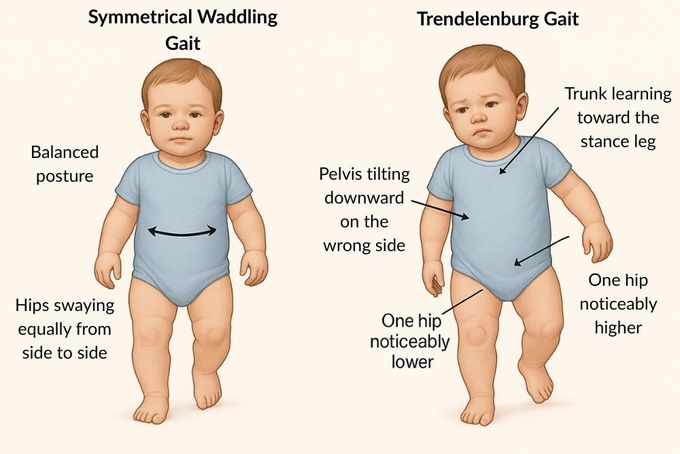
- Waddling Gait: Bilateral, symmetrical side-to-side sway in new walkers; usually resolves by age three [1].
- Trendelenburg Gait: Unilateral hip abductor weakness, pelvic drop on the opposite (swing) side and trunk lean over the stance leg. Needs evaluation [2].
What Is a Waddling Gait?
Normal waddling happens because toddlers have higher centres of gravity than older children. Their muscle control is still developing, so they use a wide stance for stability. Their hips also move side-to-side as each leg pushes forward.
The process is like learning to ride a bike. One leg moves the body forward while the other shifts weight and stabilises hip muscles. The arms stay ready at their sides, preparing for inevitable tumbles.
Waddling appears when toddlers first walk (12-18 months) and naturally fades as coordination develops, gluteal muscles strengthen, and the distance between knees decreases while standing. It's a normal part of development that typically resolves by age three as balance develops [1].
For toddlers with normal waddling, reassurance plus play-based practice is the best gait treatment.
What Is a Trendelenburg Gait?
Trendelenburg gait creates a distinctive lurching gait pattern caused by weak gluteus medius and minimus on one side [3,4]. The pelvis tilts downward on the affected side. To compensate, trunk muscles work overtime to move the body forward.
This overcompensation isn't normal development. It signals underlying medical conditions. Trendelenburg gait can appear anytime, but often shows up between ages three and twelve, though cases under two do occur.
The key difference in that side-to-side motion? Normal waddling involves both sides equally as toddlers learn balance. Trendelenburg gait shows weakness on one specific side, creating an asymmetrical lurch that won't resolve on its own.
Causes Of Waddling and Trendelenburg Gait
The timeline tells you everything about causes and treatment approaches. That's why waddling and lurching gait require different responses.
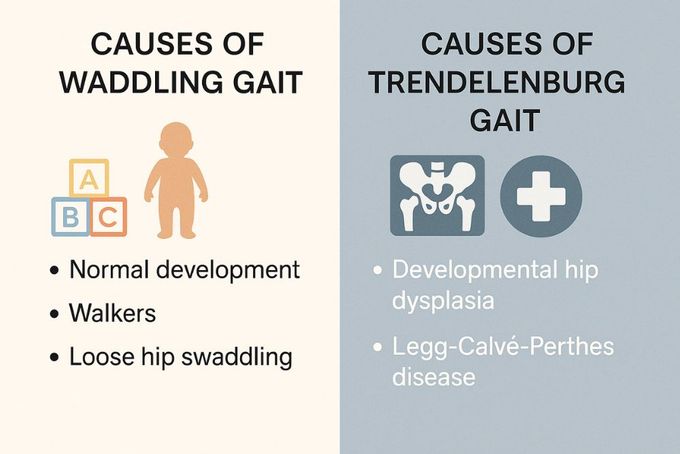
Waddling Gait Causes
For most toddlers, waddling stems from normal development. Their bodies are still figuring out this whole walking thing. The underlying anatomy reflects immature but developing muscle control.
Baby walkers can temporarily worsen the waddle [5]. While sitting in walkers, babies lean forward and walk on their toes. When they stop using them, you might notice a more prominent waddle. The situation improves as they start walking independently.
Wide-base infant carriers don't impair walking [5]. But tight swaddling around the hips can contribute to developmental hip problems. Keep swaddles loose around your baby's hips to allow free movement.
Since waddling is temporary, you should stop walker use to help your little one progress toward more agile walking. You should see gradual improvements in balance, lessening of wide-spaced stance, and development of climbing and running abilities [6].
Trendelenburg Gait Causes
Trendelenburg gait always suggests deeper medical concerns that require intervention. It stems from specific structural problems or muscle weakness.
Developmental Hip Dysplasia
Developmental hip dysplasia occurs when the hip socket doesn't form properly during fetal development [7]. The thigh bone head lacks proper "ball and socket" movement. This problem isn't visibly obvious, so doctors check for it at birth and each well visit using the Barlow and Ortolani maneuvers [8].
Treatment typically begins during the first six months of life. A Pavlik harness keeps legs and hips in an outward position, worn day and night to gradually reshape the hip socket [7]. This approach works because young infants have cartilage on bone surfaces, which can mould before the pelvic bones harden.
If the harness fails or hip dysplasia is detected after six months, a less flexible spica cast can maintain the outward leg position [7]. After 18 months, surgical reconstruction of the hip socket and thigh bone head is usually necessary [7].
Legg-Calvé-Perthes Disease
Legg-Calvé-Perthes disease happens when the blood supply to the thigh bone is lost, causing tissue death and bone loss [9].
Family history of blood-clotting disorders and secondhand smoke exposure increase the risk. Boys also have a higher chance of getting this condition than girls. Affected toddlers show downward hip tilt while lurching forward [9].
Management focuses on allowing healing time through rest and limiting activity or weight bearing on the affected leg. Ibuprofen manages hip pain. Physical therapy is the treatment standard [9].
Harnesses, casts, or braces don't work. If your little one is over six years old, a surgical reconstruction may be necessary. But rest and physical therapy heal the damaged bone in 60 per cent of cases [9].
Lurching Gait vs Waddling Gait: Diagnosis and Prevention
In a lurching gait, the pelvis drops on the swing side and the trunk leans over the stance leg; in a waddling gait, both sides sway more symmetrically. Doctors diagnose gait problems through physical exams during regular well-child visits. They assess overall health and developmental milestones.
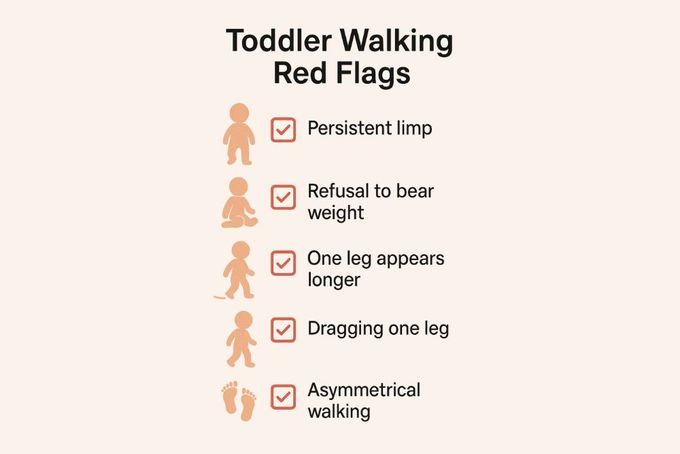
Red flags include:
- Delayed walking onset
- One leg appears longer
- Persistent limping [10]
- Refusal to bear weight
- Dragging one leg
In my clinical experience, I more often see toddlers refuse to bear weight or drag the affected leg rather than show classic Trendelenburg patterns.
X-rays diagnose Legg-Calvé-Perthes disease. Ultrasound evaluates suspected hip dysplasia in infants [11]. Because this condition is common in babies born breech, hip ultrasounds are often done before hospital discharge [12].
Prevention strategies centre on proper care. You should avoid tight swaddling around the hips to prevent hip dislocation or dysplasia. Also, don't use walkers because they create safety risks and promote a wide-spaced stance with a forward-leaning posture.
Most importantly, follow the recommended schedule for infant and toddler well visits. These occur every three months until age two, then every six months. Early detection allows for less invasive treatment strategies.
Daily Challenges and Your Role as Parent
Waddling and Trendelenburg gait have unique challenges for toddlers and different responsibilities for parents. Understanding these differences helps you respond appropriately to your little one's needs.
Waddling Gait Challenges
Normal waddling comes with predictable challenges. You should expect frequent falls since balance takes time to develop [13]. Your baby may seem clumsy or unsteady, but these issues resolve as muscle strength and coordination improve.
To set your kid on the right path, give them opportunities to increase motor skills. You can offer pull toys, balls, and seated scoot toys with wheels. Outdoor play can also teach your little one to navigate different terrains and help them strengthen the muscles necessary for coordinated walking [14].
Trendelenburg Gait Challenges
Because trunk muscles compensate for weak hip muscles, Trendelenburg gait may cause discomfort to develop after a while. It's not specifically studied in children, but adults with this condition usually have back pain [15].
Trendelenburg gait may also cause muscle weakness in the affected leg and foot [16]. Your baby may struggle to keep up with their peers in social or daycare settings. Be prepared, because they may get frustrated that they're unable to walk and run like other toddlers, causing tantrums [17].
Toddlers with Trendelenburg gait benefit from physical therapy, which can focus on strengthening the gluteus medius and minimus muscles on the affected side. You can do the recommended exercises at home.
One exercise involves having the toddler lie on the normal side, then lift the weaker leg up and outward [18]. As strength increases, you can add resistance bands. You can also do another exercise, where you kid steps side-to-side on colored squares.
For both gait types, choose shoes with flexible soles that don't restrict foot movements and materials that prevent sliding [19]. Some toddlers with Trendelenburg gait may benefit from orthotics. First Walker shoes designed to accommodate orthotics may help.
Lurching And Waddling Gait: Long-Term Outlook
Normal waddling resolves in most toddlers by age three with no lasting effects.
Long-term effects of untreated Trendelenburg gait vary based on cause. If developmental hip dysplasia goes undetected or is discovered in older children, muscle contractures and abnormal tissue formation around the hip can restrict leg movements and impair walking [20].
Friction within the hip joint can cause loss of blood supply to the thigh bone head, creating a Legg-Calvé-Perthes scenario. Reconstruction of the thigh bone head and hip socket is more successful in restoring normal gait under age four [20].
50% of children diagnosed with Legg-Calvé-Perthes develop long-term problems [9]. Pain and arthritis may develop in the affected hip after age 40.
Loss of blood supply to the thigh bone may cause flattening or growth plate damage [9]. This can cause the affected leg to grow at a different rate, resulting in leg length discrepancy.
A flattened thigh bone head can damage surrounding tissues and the hip socket, making walking more difficult.
What If Your Kid Shows Signs Of Both Gaits?
In rare cases, toddlers may show both patterns simultaneously. While waddling isn't technically a medical diagnosis, some conditions create bilateral weakness that might appear as waddling.
Duchenne Muscular Dystrophy causes weakness of the gluteal muscles on both sides [21]. Some describe the resulting walking pattern as waddling because pelvic downward motion occurs in both hips. This genetic condition causes progressive muscle fibre degeneration, becoming fatty tissue.
Calf muscles are particularly affected. Infants may have lower-than-normal muscle tone, but symptoms are more obvious after age two. This condition is also associated with learning disabilities and heart failure after age 20.
Toe-walking represents an entirely separate issue unrelated to normal waddling or Trendelenburg gait [22]. Toe-walking occurs due to foot muscle tightness in the Achilles tendons or foot muscles. Hip muscles aren't involved.
Know When to Watch and When to Act
The side-to-side walk you’re seeing could be normal waddling or a red flag. Normal waddling is symmetrical, appears when toddlers first start walking, and usually fades by age three; no treatment needed, just patience and encouragement.
Trendelenburg gait is asymmetrical, with a lurch to one side, and can signal conditions like hip dysplasia or Legg-Calvé-Perthes disease. That pattern warrants prompt medical evaluation and active treatment to protect long-term hip and mobility health.
When in doubt, trust instincts and talk to your paediatrician; early clarity beats lingering worry. If you're ready to support healthy steps at home, you can choose flexible, lightweight First Walker shoes with a wide toe box, secure closures, and slip-resistant soles.
References:
- C. Tsuyuki et al., “Estimability study on the age of toddlers’ gait development based on gait parameters,” Scientific Reports, vol. 13, no. 1, Feb. 2023, doi: 10.1038/s41598-023-30039-7. Available: https://www.nature.com/articles/s41598-023-30039-7
- T. R. T. Santos et al., “Lower limb inter-joint coordination patterns are associated with walking experience in toddlers according to limb and stance periods,” Infant Behavior and Development, vol. 68, p. 101730, Jun. 2022, doi: 10.1016/j.infbeh.2022.101730. Available: https://pubmed.ncbi.nlm.nih.gov/35714556/
- C. M. Rerucha, C. Dickison, and D. C. Baird, “Lower extremity abnormalities in children,” AAFP, Aug. 15, 2017. Available: https://www.aafp.org/pubs/afp/issues/2017/0815/p226.html
- S. Hadgaonkar and N. Mehta, “Analysis of Limp, Lurch, and List in Spinal Afflictions – What is the Root Cause?,” Journal of Orthopaedic Case Reports, vol. 13, no. 6, pp. 149–152, Jan. 2023, doi: 10.13107/jocr.2023.v13.i06.3730. Available: https://pmc.ncbi.nlm.nih.gov/articles/PMC10308978/
- P. S. C. Chagas et al., “Effects of baby walker use on the development of gait by typically developing toddlers,” Gait & Posture, vol. 76, pp. 231–237, Dec. 2019, doi: 10.1016/j.gaitpost.2019.12.013. Available: https://pubmed.ncbi.nlm.nih.gov/31874455/
- M. M. Bach et al., “Development of running is not related to time since onset of independent walking, a longitudinal case study,” Frontiers in Human Neuroscience, vol. 17, Feb. 2023, doi: 10.3389/fnhum.2023.1101432. Available: https://pmc.ncbi.nlm.nih.gov/articles/PMC9978154/
- K. Bakarman, A. M. Alsiddiky, M. Zamzam, K. O. Alzain, F. S. Alhuzaimi, and Z. Rafiq, “Developmental Dysplasia of the Hip (DDH): Etiology, diagnosis, and management,” Cureus, Aug. 2023, doi: 10.7759/cureus.43207. Available: https://pmc.ncbi.nlm.nih.gov/articles/PMC10488138/
- P. V. Samelis, “Instability testing for congenital hip dislocation: Knee extension provokes hip dislocation,” Cureus, May 2020, doi: 10.7759/cureus.8107. Available: https://pmc.ncbi.nlm.nih.gov/articles/PMC7292695/
- S. Mills and K. E. Burroughs, “Legg-Calve-Perthes Disease,” StatPearls - NCBI Bookshelf, Jul. 10, 2023. Available: https://www.ncbi.nlm.nih.gov/books/NBK513230/
- H. Raja, S. A. Khan, and A. Waheed, “The limping child — when to worry and when to refer: a GP’s guide,” British Journal of General Practice, vol. 70, no. 698, p. 467, Aug. 2020, doi: 10.3399/bjgp20x712565. Available: https://pmc.ncbi.nlm.nih.gov/articles/PMC7449436/
- A. Dessì, M. Crisafulli, E. Vannelli, and V. Fanos, “Ultrasound in developmental dysplasia of the hip: A screening study in Sardinian newborns,” Journal of Ultrasound, vol. 12, no. 2, pp. 80–84, Apr. 2009, doi: 10.1016/j.jus.2009.02.001. Available: https://pmc.ncbi.nlm.nih.gov/articles/PMC3553277/
- A. O. Rodríguez-Olivas, E. Hernández-Zamora, and E. Reyes-Maldonado, “Legg–Calvé–Perthes disease overview,” Orphanet Journal of Rare Diseases, vol. 17, no. 1, Mar. 2022, doi: 10.1186/s13023-022-02275-z. Available: https://pmc.ncbi.nlm.nih.gov/articles/PMC8922924/
- K. E. Adolph et al., “How do you learn to walk? Thousands of steps and dozens of falls per day,” Psychological Science, vol. 23, no. 11, pp. 1387–1394, Oct. 2012, doi: 10.1177/0956797612446346. Available: https://pmc.ncbi.nlm.nih.gov/articles/PMC3591461/
- D. Craig et al., “Effective Nature-Based Outdoor Play and Learning Environments for below-3 Children: A Literature-Based Summary,” International Journal of Environmental Research and Public Health, vol. 21, no. 9, p. 1247, Sep. 2024, doi: 10.3390/ijerph21091247. Available: https://pmc.ncbi.nlm.nih.gov/articles/PMC11432191/
- G. Z. Pizol, K. F. M. Franco, G. C. Miyamoto, and C. M. N. Cabral, “Is there hip muscle weakness in adults with chronic non-specific low back pain? A cross-sectional study,” BMC Musculoskeletal Disorders, vol. 24, no. 1, Oct. 2023, doi: 10.1186/s12891-023-06920-x. Available: https://pubmed.ncbi.nlm.nih.gov/37805476/
- “Applications of gait analysis in pediatric orthopaedics.” Available: https://www.researchgate.net/publication/303530154_Applications_of_gait_analysis_in_pediatric_orthopaedics
- W. A. Marquis, A. N. Noroña, and B. L. Baker, “Developmental delay and emotion dysregulation: Predicting parent–child conflict across early to middle childhood.,” Journal of Family Psychology, vol. 31, no. 3, pp. 327–335, Jan. 2017, doi: 10.1037/fam0000267. Available: https://pmc.ncbi.nlm.nih.gov/articles/PMC5378638/
- V. N. Gandbhir, J. C. Lam, F. Lui, and A. Rayi, “Trendelenburg Gait,” StatPearls - NCBI Bookshelf, Feb. 29, 2024. Available: https://www.ncbi.nlm.nih.gov/books/NBK541094/
- S. Cranage, L. Perraton, K. Bowles, and C. Williams, “The impact of shoe flexibility on gait, pressure and muscle activity of young children. A systematic review,” Journal of Foot and Ankle Research, vol. 12, no. 1, Jan. 2019, doi: 10.1186/s13047-019-0365-7. Available: https://doi.org/10.1186/s13047-019-0365-7
- Ö. Çiçekli and M. Doğan, “Evaluation of surgical outcome in advanced age patients with developmental hip dysplasia,” International Journal of Surgery, vol. 52, pp. 44–49, Feb. 2018, doi: 10.1016/j.ijsu.2018.02.020. Available: https://pubmed.ncbi.nlm.nih.gov/29455046/
- I. Vandekerckhove et al., “Gait classification for growing children with Duchenne muscular dystrophy,” Scientific Reports, vol. 14, no. 1, May 2024, doi: 10.1038/s41598-024-61231-y. Available: https://www.nature.com/articles/s41598-024-61231-y
- R. Engelbert, J. W. Gorter, C. Uiterwaal, E. Van De Putte, and P. Helders, “Idiopathic toe-walking in children, adolescents and young adults: a matter of local or generalised stiffness?,” BMC Musculoskeletal Disorders, vol. 12, no. 1, Mar. 2011, doi: 10.1186/1471-2474-12-61. Available: https://pmc.ncbi.nlm.nih.gov/articles/PMC3070692/
Disclaimer: First Walkers' information is intended for educational and informational purposes related to toddler footwear and feet. We encourage you to consider individual circumstances and consult qualified orthopaedists about specific conditions.
FAQs
What is another name for Trendelenburg gait?
Abductor lurch (aka gluteus medius lurch).
What is another name for a waddling gait?
Myopathic gait.
How to identify Trendelenburg gait?
When your little one stands on the affected leg, the pelvis drops on the opposite side, and the trunk leans toward the stance side.
What is a normal gait called?
Normal (physiologic) gait.